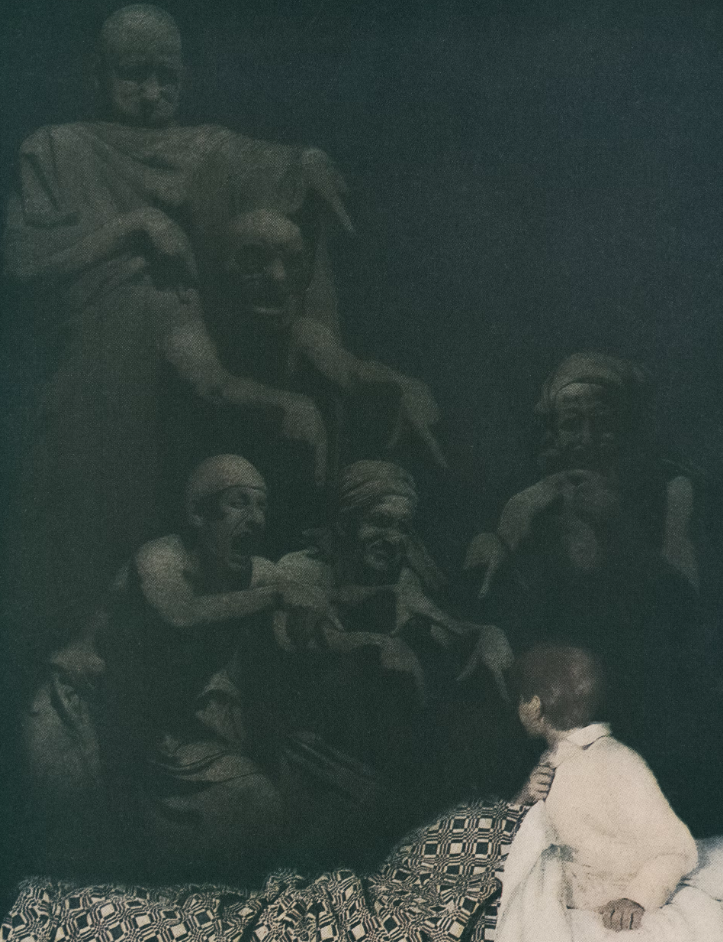
Visual hallucinations, bizarre delusions, violent behaviour, and disorganised speech often dominate media portrayals of Schizophrenia (Owen, 2012), raising intrigue about a disorder that seemingly pulls someone away from our shared understanding of reality. The stereotyped depictions may seem like an “obvious” fantasy, but to an individual experiencing these symptoms, the delusions and hallucinations feel intensely real. Rather than fantasy being a choice or form of escape, like with movies or literature, for those with schizophrenia, it is something they are compelled to live within – creating a tension between a personal fantasy world and the external shared reality. This raises a deeper question: how do we define reality?
Visual hallucinations, bizarre delusions, violent behaviour, and disorganised speech often dominate media portrayals of Schizophrenia (Owen, 2012), raising intrigue about a disorder that seemingly pulls someone away from our shared understanding of reality. The stereotyped depictions may seem like an “obvious” fantasy, but to an individual experiencing these symptoms, the delusions and hallucinations feel intensely real. Rather than fantasy being a choice or form of escape, like with movies or literature, for those with schizophrenia, it is something they are compelled to live within – creating a tension between a personal fantasy world and the external shared reality. This raises a deeper question: how do we define reality?
Photo by The New York Public Library
Photo by The New York Public Library
Schizophrenia is a severe mental illness that profoundly alters the way a person thinks, feels, and behaves, leading to an apparent loss of sense of reality. It holds immense stigma and is often oversimplified or stereotyped as “going crazy” and “hearing voices”, but in reality, the disorder is far more complex and pervasive. It distorts perceptions, warps thoughts, and disrupts emotions and cognitions, making the familiar world feel foreign and confusing. To address the stigma and stereotypes around this disorder, it is crucial to explore how schizophrenia is viewed clinically, personally, and in terms of treatment approaches. In general, schizophrenia challenges our understanding of reality by meddling in what we consider to be shared perception, forcing us to reconsider the subjective nature of what we call “reality”.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) categorises schizophrenia in the chapter “Schizophrenia Spectrum and Other Psychotic Disorders”. This chapter includes a variety of disorders that share a defining feature of psychosis (American Psychiatric Association, 2013). Psychosis, or a psychotic episode, is characterised by a loss of contact with reality through hallucinations, delusions, and/or disorganised behaviour or speech (NHS, 2023). While psychosis has a lifetime prevalence of approximately 5-7% (Staines et al., 2022), schizophrenia is less common, affecting around 0.4% of the global population (World Health Organization, 2022). To be diagnosed with schizophrenia, an individual must exhibit at least two of the core symptoms: hallucinations, delusions, disorganised speech, grossly disorganised behaviour, or negative symptoms like reduced emotional expression or lack of motivation. Schizophrenia symptoms are further divided into positive and negative symptoms. Positive symptoms – such as hallucinations, delusions, and disorganised behaviour – add to the individual’s sense of reality by creating experiences that previously did not exist. In contrast, negative symptoms, such as diminished emotional expression and avolition, detract from the individuals’ reality by making them more withdrawn and reducing their ability to engage socially. Exploring qualitative research and personal accounts of schizophrenia can offer valuable insight into the confusing disorder and its symptoms – and importantly, a glimpse into their reality.
“Schizophrenia challenges our understanding of reality by meddling in what we consider to be shared perception, forcing us to reconsider the subjective nature of what we call “reality”.”
Hallucinations are vivid and clear sensory experiences that occur outside of voluntary control and without any external stimulus. While hallucinations can affect any sensory modality, auditory hallucinations are the most prevalent in schizophrenia (American Psychiatric Association, 2013, p. 103). Lee (2020), in his personal account of auditory verbal hallucinations, describes how they occur sporadically, often in response to heightened stress, and this awareness helps him manage them. Additionally, being told that his disease was incurable felt disheartening, but also allowed him to come to terms with his sensory experiences with less shock and improved personal care. Through learning more about his mental illness and dedicating time to self-discovery, he was able to start viewing the voices not as threatening or peculiar, but rather as a response to his current state of mind or external circumstances. This contributes to the idea that the subjective reality of positive symptoms need not be rejected immediately, but also require immense care and insight so as to not allow them to negatively dominate one’s life. Delusions, on the other hand, pertain to fixed beliefs – across a variety of themes – that remain unchanged despite contrary evidence. Persecutory delusions, where an individual believes they are being harmed or targeted, and delusions of reference, where they feel that everyday occurrences are directed at them, are the most common types. According to Cambridge University Press’ Psychiatric Bulletin (2018), first-person accounts suggest that delusions arise gradually in onset, accompanied by fear and odd moods, but also require very gradual and slow debunking throughout treatment, with immense social support for ideal outcomes. Hence, delusions are not merely irrational thoughts, but carry emotional weight and take substantial time to build and become full-fledged and difficult to dismantle.
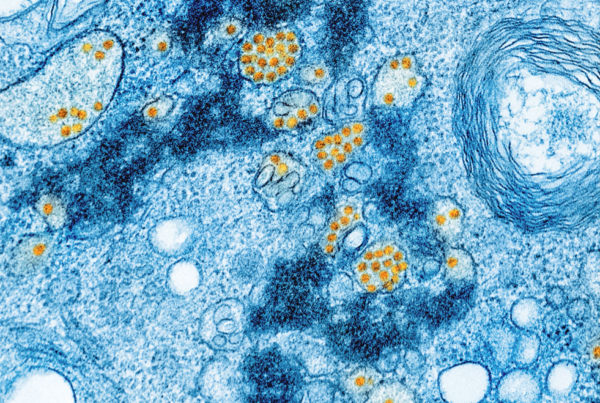
It may be easy to assume that individuals suffering from auditory hallucinations or delusions of persecution or grandeur are detached from reality, but these experiences feel profoundly real to them. Neuropsychological research provides evidence of altered sensory processing and cognitive differences in people with schizophrenia (Luvsannyam et al., 2022). Moreover, there is evidence that erroneous perceptions may arise from interactions between altered top-down and bottom-up processes in the brain (Allen, et al., 2008), supporting the realness of the subjective reality of those with schizophrenia. Thus, while their experiences may seem far from our shared social reality, dismissing them as mere “fantasy” can invalidate their experience and perpetuate the stigma by increasing the mysticism around the mental illness.
Despite the altered personal realities they experience, individuals with schizophrenia still have to navigate a complex society that demands certain behavioural standards – whether at work or during everyday tasks like grocery shopping. Coping with societal reality and expectations is what schizophrenia treatment targets. Though the disorder is considered incurable, it is better understood as a lifelong process that can be managed with medication and therapy (Johns Hopkins Medicine, 2024). Essentially, treatment attempts to neutralise their version of reality. The first line of treatment is antipsychotic medication, which works to reduce positive symptoms like hallucinations, delusions and disorganised symptoms (Johns Hopkins Medicine, 2024). However, many patients view medication as disconnecting them from their internal world, leading to treatment adherence issues; which can be scary in itself (Cambridge University Press, 2018). Despite these difficulties, medication can bring peace to patients and their families, improving their overall social support system (Jameel et al., 2020).
“It may be easy to assume that individuals suffering from auditory hallucinations or delusions of persecution or grandeur are detached from reality, but these experiences feel profoundly real to them.”
Schizophrenia presents significant treatment challenges due to difficulties in connecting with patients, poor treatment adherence, and the functional impairments that result (Mucci, et al., 2020). Clinicians also face barriers, such as misunderstandings of their role, providing inadequate descriptions of the condition, and potential biases or stigmas (Hasson-Ohayon et al., 2017). Developing a strong therapeutic alliance, i.e. a therapist-patient collaboration, is particularly difficult, as rejecting the patient’s reality outright may hinder progress, requiring clinicians to navigate a fine line in treatment. Research emphasises that the therapeutic alliance transcends specific treatment features in improving patient outcomes (Stubbe, 2018), making time dedicated to building this connection crucial. Improving psychoeducation, a concept often neglected in schizophrenia, has been proposed to serve as a model for shared understanding – or reality – between the clinician and client (Herrera et al., 2023). In considering these aspects, the very nature of reality becomes central to treatment, as both the clinician and patient must create a shared reality that acknowledges subjective experiences while working towards functioning in a complex societal external world. Ultimately, it is important to be careful with the language used among such patients, as it is not just to claim (from a high horse) that they are removed from reality, as this lacks the necessary nuance and respect towards people who experience these symptoms as extremely real, often scary, and traumatic.
Overall, Schizophrenia challenges our understanding of reality by blurring the line between subjective and shared perceptions. Exploring and treating these realities requires empathy, respect, and a deeper understanding of the complexities of the human mind. Ultimately, schizophrenia is an extremely complex disorder that requires immense patience and comprehensive understanding. Not exploring an individual’s reality as inherently “fake” but rather a lived experience may be key to fostering better outcomes and reducing the stigma surrounding the illness.
To read more on the specific experiences of people with schizophrenia based on two books written about it, please refer to Annabel Simjouw’s article on the Spiegeloog website titled, “Writing about Schizophrenia”. <<
References
- Allen, P., Larøi, F., McGuire, P. K., & Aleman, A. (2007). The hallucinating brain: A review of structural and functional neuroimaging studies of hallucinations. Neuroscience & Biobehavioral Reviews, 32(1), 175–191. https://doi.org/10.1016/j.neubiorev.2007.07.012
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th
- ed.). https://doi.org/10.1176/appi.books.9780890425596
- Hasson‐Ohayon, I., Kravetz, S., & Lysaker, P. H. (2016). The Special Challenges of Psychotherapy with Persons with Psychosis: Intersubjective Metacognitive Model of Agreement and Shared Meaning. Clinical Psychology & Psychotherapy, 24(2), 428–440. https://doi.org/10.1002/cpp.2012
- Herrera, S. N., Sarac, C., Phili, A., Gorman, J., Martin, L., Lyallpuri, R., Dobbs, M. F., DeLuca, J. S., Mueser, K. T., Wyka, K. E., Yang, L. H., Landa, Y., & Corcoran, C. M. (2023). Psychoeducation for individuals at clinical high risk for psychosis: A scoping review. Schizophrenia Research, 252, 148–158. https://doi.org/10.1016/j.schres.2023.01.008
- Jameel, H. T., Panatik, S. A., Nabeel, T., Sarwar, F., Yaseen, M., Jokerst, T., & Faiz, Z. (2020). Observed social support and willingness for the treatment of patients with schizophrenia. Psychology Research and Behavior Management,
- Johns Hopkins Medicine. (2024). Schizophrenia. Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/schizophrenia#:~:text=How%20is%20schizophrenia%20treated%3F,managed%20with%20medicine%20and%20therapy
- Luvsannyam, E., Jain, M. S., Pormento, M. K. L., Siddiqui, H., Balagtas, A. R. A., Emuze, B. O., & Poprawski, T. (2022). Neurobiology of Schizophrenia: A Comprehensive Review. Cureus. https://doi.org/10.7759/cureus.23959
- Mucci, A., Kawohl, W., Maria, C., & Wooller, A. (2020). Treating schizophrenia: Open conversations and stronger relationships through psychoeducation and shared Decision-Making. Frontiers in Psychiatry, 11. https://doi.org/10.3389/fpsyt.2020.00761
- NHS. (2023). Overview – Psychosis. NHS. https://www.nhs.uk/mental-health/conditions/psychosis/overview/
- Owen, P. R. (2012). Portrayals of schizophrenia by Entertainment Media: A content analysis of contemporary movies. Psychiatric Services, 63(7), 655–659. https://doi.org/10.1176/appi.ps.201100371
- Sheikh, Z. (2024). Schizophrenia onset: When do symptoms usually start? WebMD.
- https://www.webmd.com/schizophrenia/schizophrenia-onset-symptoms
- Staines, L., Healy, C., Coughlan, H., Clarke, M., Kelleher, I., Cotter, D., & Cannon, M. (2022). Psychotic experiences in the general population, a review; definition, risk factors, outcomes and interventions. Psychological Medicine, 52(15), 3297–3308. https://doi.org/10.1017/s0033291722002550
- Stubbe, D. E. (2018). The therapeutic alliance: the fundamental element of psychotherapy. FOCUS
- the Journal of Lifelong Learning in Psychiatry, 16(4), 402–403.
- https://doi.org/10.1176/appi.focus.20180022
- World Health Organization. (2022). Schizophrenia. https://www.who.int/news-room/fact-sheets/detail/schizophrenia#:~:text=Schizophrenia%20affects%20approximately%2024%20million,as%20many%20other%20mental%20disorders
Schizophrenia is a severe mental illness that profoundly alters the way a person thinks, feels, and behaves, leading to an apparent loss of sense of reality. It holds immense stigma and is often oversimplified or stereotyped as “going crazy” and “hearing voices”, but in reality, the disorder is far more complex and pervasive. It distorts perceptions, warps thoughts, and disrupts emotions and cognitions, making the familiar world feel foreign and confusing. To address the stigma and stereotypes around this disorder, it is crucial to explore how schizophrenia is viewed clinically, personally, and in terms of treatment approaches. In general, schizophrenia challenges our understanding of reality by meddling in what we consider to be shared perception, forcing us to reconsider the subjective nature of what we call “reality”.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) categorises schizophrenia in the chapter “Schizophrenia Spectrum and Other Psychotic Disorders”. This chapter includes a variety of disorders that share a defining feature of psychosis (American Psychiatric Association, 2013). Psychosis, or a psychotic episode, is characterised by a loss of contact with reality through hallucinations, delusions, and/or disorganised behaviour or speech (NHS, 2023). While psychosis has a lifetime prevalence of approximately 5-7% (Staines et al., 2022), schizophrenia is less common, affecting around 0.4% of the global population (World Health Organization, 2022). To be diagnosed with schizophrenia, an individual must exhibit at least two of the core symptoms: hallucinations, delusions, disorganised speech, grossly disorganised behaviour, or negative symptoms like reduced emotional expression or lack of motivation. Schizophrenia symptoms are further divided into positive and negative symptoms. Positive symptoms – such as hallucinations, delusions, and disorganised behaviour – add to the individual’s sense of reality by creating experiences that previously did not exist. In contrast, negative symptoms, such as diminished emotional expression and avolition, detract from the individuals’ reality by making them more withdrawn and reducing their ability to engage socially. Exploring qualitative research and personal accounts of schizophrenia can offer valuable insight into the confusing disorder and its symptoms – and importantly, a glimpse into their reality.
“Schizophrenia challenges our understanding of reality by meddling in what we consider to be shared perception, forcing us to reconsider the subjective nature of what we call “reality”.”
Hallucinations are vivid and clear sensory experiences that occur outside of voluntary control and without any external stimulus. While hallucinations can affect any sensory modality, auditory hallucinations are the most prevalent in schizophrenia (American Psychiatric Association, 2013, p. 103). Lee (2020), in his personal account of auditory verbal hallucinations, describes how they occur sporadically, often in response to heightened stress, and this awareness helps him manage them. Additionally, being told that his disease was incurable felt disheartening, but also allowed him to come to terms with his sensory experiences with less shock and improved personal care. Through learning more about his mental illness and dedicating time to self-discovery, he was able to start viewing the voices not as threatening or peculiar, but rather as a response to his current state of mind or external circumstances. This contributes to the idea that the subjective reality of positive symptoms need not be rejected immediately, but also require immense care and insight so as to not allow them to negatively dominate one’s life. Delusions, on the other hand, pertain to fixed beliefs – across a variety of themes – that remain unchanged despite contrary evidence. Persecutory delusions, where an individual believes they are being harmed or targeted, and delusions of reference, where they feel that everyday occurrences are directed at them, are the most common types. According to Cambridge University Press’ Psychiatric Bulletin (2018), first-person accounts suggest that delusions arise gradually in onset, accompanied by fear and odd moods, but also require very gradual and slow debunking throughout treatment, with immense social support for ideal outcomes. Hence, delusions are not merely irrational thoughts, but carry emotional weight and take substantial time to build and become full-fledged and difficult to dismantle.
It may be easy to assume that individuals suffering from auditory hallucinations or delusions of persecution or grandeur are detached from reality, but these experiences feel profoundly real to them. Neuropsychological research provides evidence of altered sensory processing and cognitive differences in people with schizophrenia (Luvsannyam et al., 2022). Moreover, there is evidence that erroneous perceptions may arise from interactions between altered top-down and bottom-up processes in the brain (Allen, et al., 2008), supporting the realness of the subjective reality of those with schizophrenia. Thus, while their experiences may seem far from our shared social reality, dismissing them as mere “fantasy” can invalidate their experience and perpetuate the stigma by increasing the mysticism around the mental illness.
Despite the altered personal realities they experience, individuals with schizophrenia still have to navigate a complex society that demands certain behavioural standards – whether at work or during everyday tasks like grocery shopping. Coping with societal reality and expectations is what schizophrenia treatment targets. Though the disorder is considered incurable, it is better understood as a lifelong process that can be managed with medication and therapy (Johns Hopkins Medicine, 2024). Essentially, treatment attempts to neutralise their version of reality. The first line of treatment is antipsychotic medication, which works to reduce positive symptoms like hallucinations, delusions and disorganised symptoms (Johns Hopkins Medicine, 2024). However, many patients view medication as disconnecting them from their internal world, leading to treatment adherence issues; which can be scary in itself (Cambridge University Press, 2018). Despite these difficulties, medication can bring peace to patients and their families, improving their overall social support system (Jameel et al., 2020).
“It may be easy to assume that individuals suffering from auditory hallucinations or delusions of persecution or grandeur are detached from reality, but these experiences feel profoundly real to them.”
Schizophrenia presents significant treatment challenges due to difficulties in connecting with patients, poor treatment adherence, and the functional impairments that result (Mucci, et al., 2020). Clinicians also face barriers, such as misunderstandings of their role, providing inadequate descriptions of the condition, and potential biases or stigmas (Hasson-Ohayon et al., 2017). Developing a strong therapeutic alliance, i.e. a therapist-patient collaboration, is particularly difficult, as rejecting the patient’s reality outright may hinder progress, requiring clinicians to navigate a fine line in treatment. Research emphasises that the therapeutic alliance transcends specific treatment features in improving patient outcomes (Stubbe, 2018), making time dedicated to building this connection crucial. Improving psychoeducation, a concept often neglected in schizophrenia, has been proposed to serve as a model for shared understanding – or reality – between the clinician and client (Herrera et al., 2023). In considering these aspects, the very nature of reality becomes central to treatment, as both the clinician and patient must create a shared reality that acknowledges subjective experiences while working towards functioning in a complex societal external world. Ultimately, it is important to be careful with the language used among such patients, as it is not just to claim (from a high horse) that they are removed from reality, as this lacks the necessary nuance and respect towards people who experience these symptoms as extremely real, often scary, and traumatic.
Overall, Schizophrenia challenges our understanding of reality by blurring the line between subjective and shared perceptions. Exploring and treating these realities requires empathy, respect, and a deeper understanding of the complexities of the human mind. Ultimately, schizophrenia is an extremely complex disorder that requires immense patience and comprehensive understanding. Not exploring an individual’s reality as inherently “fake” but rather a lived experience may be key to fostering better outcomes and reducing the stigma surrounding the illness.
To read more on the specific experiences of people with schizophrenia based on two books written about it, please refer to Annabel Simjouw’s article on the Spiegeloog website titled, “Writing about Schizophrenia”. <<
References
- Allen, P., Larøi, F., McGuire, P. K., & Aleman, A. (2007). The hallucinating brain: A review of structural and functional neuroimaging studies of hallucinations. Neuroscience & Biobehavioral Reviews, 32(1), 175–191. https://doi.org/10.1016/j.neubiorev.2007.07.012
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th
- ed.). https://doi.org/10.1176/appi.books.9780890425596
- Hasson‐Ohayon, I., Kravetz, S., & Lysaker, P. H. (2016). The Special Challenges of Psychotherapy with Persons with Psychosis: Intersubjective Metacognitive Model of Agreement and Shared Meaning. Clinical Psychology & Psychotherapy, 24(2), 428–440. https://doi.org/10.1002/cpp.2012
- Herrera, S. N., Sarac, C., Phili, A., Gorman, J., Martin, L., Lyallpuri, R., Dobbs, M. F., DeLuca, J. S., Mueser, K. T., Wyka, K. E., Yang, L. H., Landa, Y., & Corcoran, C. M. (2023). Psychoeducation for individuals at clinical high risk for psychosis: A scoping review. Schizophrenia Research, 252, 148–158. https://doi.org/10.1016/j.schres.2023.01.008
- Jameel, H. T., Panatik, S. A., Nabeel, T., Sarwar, F., Yaseen, M., Jokerst, T., & Faiz, Z. (2020). Observed social support and willingness for the treatment of patients with schizophrenia. Psychology Research and Behavior Management,
- Johns Hopkins Medicine. (2024). Schizophrenia. Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/schizophrenia#:~:text=How%20is%20schizophrenia%20treated%3F,managed%20with%20medicine%20and%20therapy
- Luvsannyam, E., Jain, M. S., Pormento, M. K. L., Siddiqui, H., Balagtas, A. R. A., Emuze, B. O., & Poprawski, T. (2022). Neurobiology of Schizophrenia: A Comprehensive Review. Cureus. https://doi.org/10.7759/cureus.23959
- Mucci, A., Kawohl, W., Maria, C., & Wooller, A. (2020). Treating schizophrenia: Open conversations and stronger relationships through psychoeducation and shared Decision-Making. Frontiers in Psychiatry, 11. https://doi.org/10.3389/fpsyt.2020.00761
- NHS. (2023). Overview – Psychosis. NHS. https://www.nhs.uk/mental-health/conditions/psychosis/overview/
- Owen, P. R. (2012). Portrayals of schizophrenia by Entertainment Media: A content analysis of contemporary movies. Psychiatric Services, 63(7), 655–659. https://doi.org/10.1176/appi.ps.201100371
- Sheikh, Z. (2024). Schizophrenia onset: When do symptoms usually start? WebMD.
- https://www.webmd.com/schizophrenia/schizophrenia-onset-symptoms
- Staines, L., Healy, C., Coughlan, H., Clarke, M., Kelleher, I., Cotter, D., & Cannon, M. (2022). Psychotic experiences in the general population, a review; definition, risk factors, outcomes and interventions. Psychological Medicine, 52(15), 3297–3308. https://doi.org/10.1017/s0033291722002550
- Stubbe, D. E. (2018). The therapeutic alliance: the fundamental element of psychotherapy. FOCUS
- the Journal of Lifelong Learning in Psychiatry, 16(4), 402–403.
- https://doi.org/10.1176/appi.focus.20180022
- World Health Organization. (2022). Schizophrenia. https://www.who.int/news-room/fact-sheets/detail/schizophrenia#:~:text=Schizophrenia%20affects%20approximately%2024%20million,as%20many%20other%20mental%20disorders